ADHD Information
What is ADHD?
ADHD (Attention-Deficit Hyperactivity Disorder) is a neuro-developmental condition that affects how the brain manages:
Attention
Activity levels
Impulse control
‘Neuro’ = nerves and nervous system) ‘
‘Developmental’ = the development of the brain and nervous system)
ADHD is a neurodevelopmental condition which affects how the brain is developed and wired.
These structural differences affect focus, memory, learning and emotions.
ADHD is present from childhood, rather than something that develops later in life (though many people arent diagnosed until adulthood).
Mental health conditions are illnesses that develop later in life (and often influenced by biopsychosocial factors)
ADHD does not equal mental illness. However, people with ADHD are more likely to develop mental health conditions.
ADHD is related to how the brain is wired (neurodevelopmental) rather than an illness that develops later (mental illness)
Neurodevelopmental Disorders (like ADHD) and Mental Health Disorders are different.
ADHD = Mental Illness
Why ADHD Occurs:
ADHD often runs in families - research shows strong heritability.
Brain scans highlight differences in areas that manage focus, planning, and self-control.
Brain chemicals (like dopamine and norepinephrine) work differently, which affects motivation and attention.
Strong genetic component
Structural differences in the brain
Neurochemical differences
ADHD Symptoms
ADHD shows up in three main clusters:
Inattention – distracted, forgetful, disorganised, struggle to start and finish tasks
Hyperactivity – restless, fidgety, “on the go”, diffiuclty staying still, hard to relax, feeling driven by a motor.
Impulsivity – interrupting, blurting things out, acting before thinking, diffiuclty waiting.
People may predominately experience inattentive symptoms, some predominantly hyperactive symptoms but many experience a combination
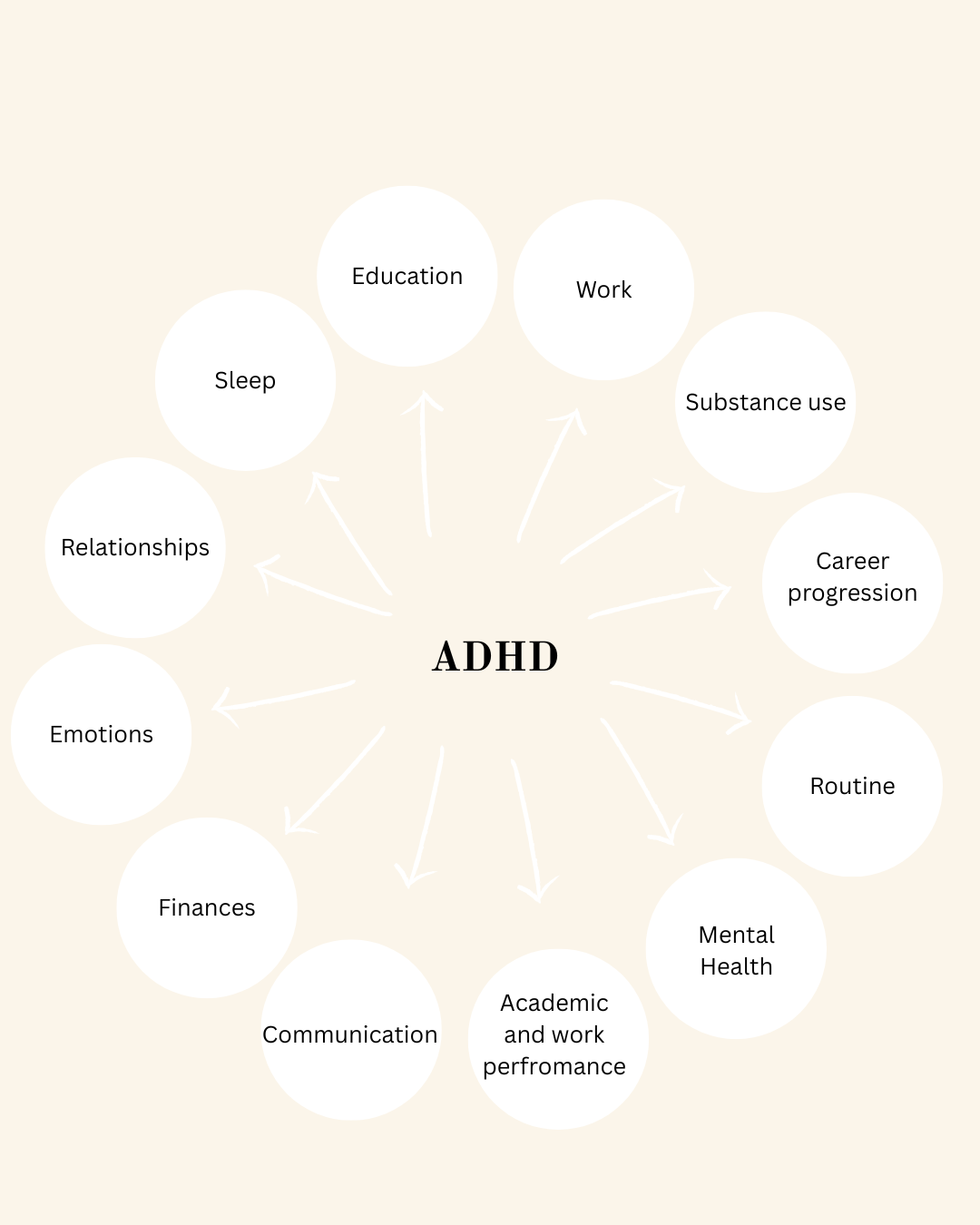
ADHD Impact - more than just a concentration and memory problem
What Makes ADHD Worse?
While ADHD is lifelong, certain patterns can make symptoms worse and harder to manage
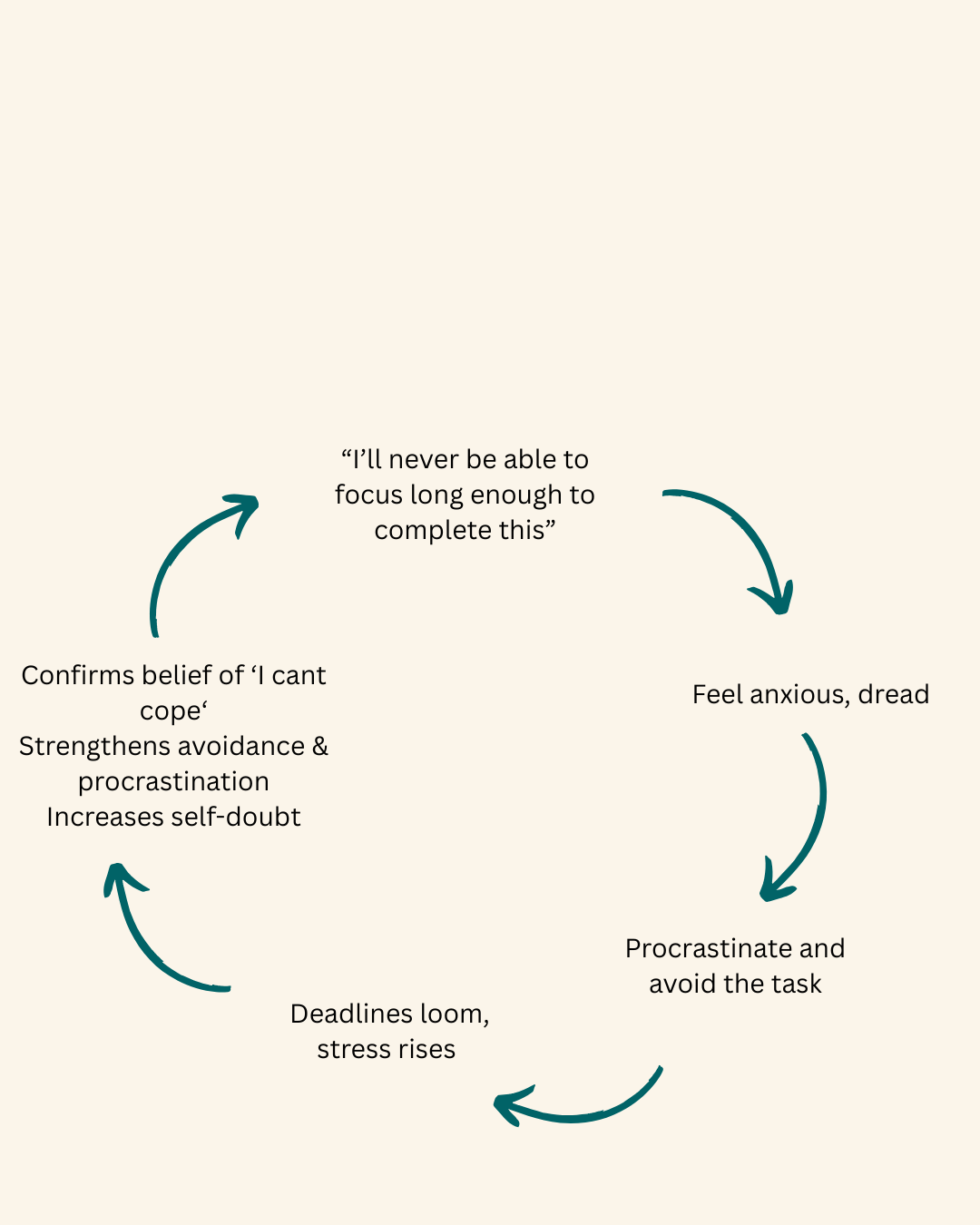
Avoidance and procrastination →accumulates problems, increases pressure and reduces confidence.
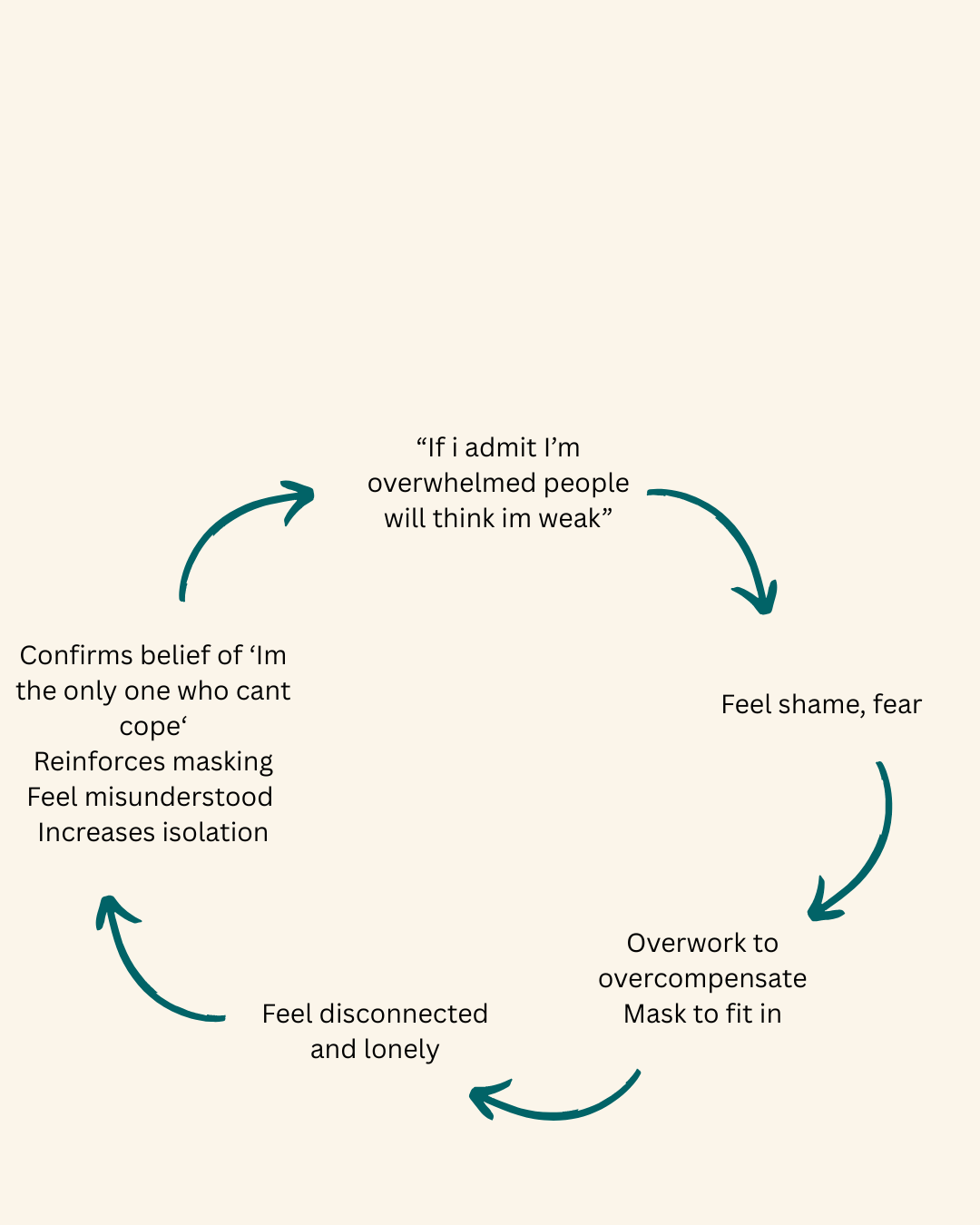
Negative self-talk and shame → reinforces negative beliefs of self.
Burnout cycles →periods of overworking followed by exhuastion, leads to inconsistent performance, tendency to gravitate to other unhelpful behaviours.
Unrealistic expectations → increases shame, fuels low self confidence.
Poor sleep → worsens focus, mood, and impulse control.
Lack of structure or routine → harder for the brain to regulate focus and energy.
Lack of understanding or support from others → creates isolation, increases self-blame.
Stress and anxiety → competing for mental resources, making ADHD symptoms stronger.
These maintenance cycles can keep people stuck and make life feel harder. Breaking them with the right strategies is a key part of therapy.
What Helps ADHD
ADHD is treatable and can be managed. Support works best when it’s tailored to you:
Therapy – works coping skills, self-esteem, anxiety, shame, and emotional challenges.
Medication – helps balance brain chemistry, improving focus and impulse control easier.
Coaching skills – gives practical tools for organisation, planning, and follow-through.
Lifestyle + Environment changes – setting things up so your brain works with your systems, not against them.
With the right support, people with ADHD don’t just cope or get by in survival mode — they can thrive.
Therapy for ADHD - Tailored to You
Therapy isn’t one-size-fits-all — especially with ADHD.
Standard CBT isnt always designed with ADHD in mind, and you shouldn’t have to mask or force yourself into a model that doesn’t fit.
I offer ADHD-adapted therapy based on evidence-based treatment and research that works with the ADHD, not against it.
My approach blends CBT with other research-backed therapies and approaches to create a bespoke and tailored treatment plan built around your specific needs, goals and challenges - whether that’s focusing on your ADHD or any accompanying challenges such as anxiety, low self-esteem, or perfectionism.
Together, we’ll identify the patterns keeping you stuck and develop strategies that actually work for your brain, so you can break cycles, understand yourself and feel equipped with strategies that work for you.
Read more about therapy for ADHD or my approach below: